The Council for Medical Schemes (CMS) says it has witnessed a resurgence in complaints against medical schemes and administrators that claw back losses allegedly incurred by healthcare professionals because of fraud, waste, and abuse (FWA).
The CMS last week released its annual report for the 2023/24 financial year. The statutory body regulates and supervises the country’s 16 open and 55 restricted (closed) registered medical schemes and 34 administrators (including self-administered schemes and limited accreditation administrators).
A section of the report is devoted to an analysis of the complaints received by the regulator’s Complaints Adjudication Unit.
According to the report, there was a “short respite” in complaints about FWA following the release of the Section 59 Inquiry Panel’s interim report. Section 59 of the Medical Schemes Act (MSA) authorises schemes to recover money paid to healthcare practitioners where those amounts were claimed unlawfully.
In 2019, the CMS launched an investigation into claims by members of Solutionist Thinkers and the National Health Care Professionals Association that black medical professionals were treated unfairly.
The Inquiry Panel’s interim report, which was released in January 2021, found that some medical schemes racially profiled black healthcare practitioners so that they did not enjoy the same benefits as other races when claiming for healthcare services.
But there has been a resurgence in these complaints, which, the CMS says, are often the result of disputes over coding interpretation, scope of practice disagreements, and allegations of overservicing and claiming for services not rendered.
“Healthcare providers criticise the lack of fairness in the claims audit conducted by medical schemes, as well as the methodology applied in quantifying the extent of the alleged losses. On the other hand, medical schemes argue that members’ funds are being depleted by the ongoing scourge of FWA,” the Council says.
The CMS says it continues to adjudicate these matters while awaiting the release of the panel’s final report.
In June, the CMS said the final report was “close to completion and will be released and published as soon as possible”.
Other complaint trends
The annual report also drew attention to the following complaint trends:
Beneficiaries don’t understand the terms used
Beneficiaries do not understand concepts commonly used in the medical scheme industry. Terms such as pre-authorisation, treatment protocols, formularies, and scheme tariffs seem to confuse beneficiaries.
The CMS recommends that medical schemes and brokers dedicate time and effort to explain these terms in simple, understandable language.
Non-payment and short payment of claims
The CMS says it remains concerned by disputes where beneficiaries incur out-of-pocket payments because of the non-payment and/or short payment of claims.
In some instances, beneficiaries were unduly denied benefits to which they were entitled, and the CMS correctly ruled in favour of the complainants.
However, there were a substantial number of complaints where medical schemes had correctly applied the Act and the rules. In these cases, rulings were issued against complainants, and it became apparent that their understanding of benefit rules and limits was still lacking.
The CMS says it is important that beneficiaries familiarise themselves with the level of coverage purchased and ensure that the chosen benefit option matches their healthcare needs.
Beneficiaries should read and understand the rules governing their benefit options, and where they encounter difficulties, they must contact their scheme before incurring unplanned costs.
Medical schemes must ensure that benefit options are simplified and communicated in clear and understandable language. Communication channels must also be kept open and accessible to beneficiaries, the CMS says.
Lack of response to complaints
Another concern was the increase in complaints where medical schemes failed to address member queries until they were escalated to the regulator as complaints.
The CMS also noted a trend of schemes not informing members of their internal dispute resolution and clinical appeal processes.
The MSA and its Regulations oblige medical schemes to implement query escalation processes where members’ funding and benefit queries can be timely addressed.
Incorrect limits on PMB funding
Despite issuing numerous rulings against offending medical schemes, the CMS says it continued to see complaints where schemes incorrectly applied monetary caps and benefit limits to PMB funding for post-amputation prosthetic limbs.
The CMS says its rulings have clarified the correct interpretation of Explanatory Note 2 to the Regulations, which schemes were using to limit funding based on what they perceived to be the cost at public sector facilities.
The regulator says it is monitoring the incorrect use of Explanatory Note 2, and it expects that offending schemes will rectify this conduct.
Decrease in the number of complaints
The Complaints Adjudication Unit received and resolved fewer complaints in 2023/24 than it did in the previous financial year.
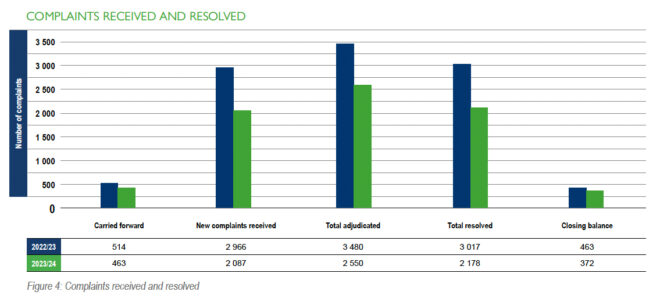
The overall number of complaints investigated in 2023/24 was 2 550 (2022/23: 3 480), which included 463 (514) complaints carried over from the previous financial year and 2 087 (2 966) newly registered complaints.
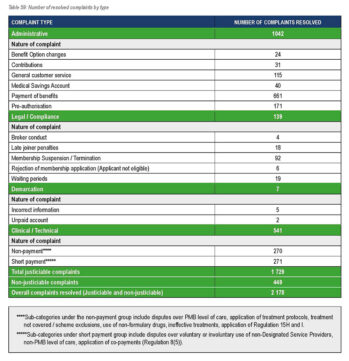
During the year under review, 2 178 complaints were resolved. This includes 1 729 Category 1 and Category 2 complaints, as well as 449 non-justiciable complaints.
Category 1 complaints are uncomplicated but may require referrals for inputs from the CMS or externally.
Category 2 complaints are clinically and/or legally complex, requiring extensive investigation, the collation of evidence, and referrals for inputs from the CMS and externally.
Non-justiciable complaints do not meet the requirements of a complaint as set out in section 1 of the MSA. This classification also includes complaints where there is insufficient or no supporting evidence, as well as duplicate complaints.
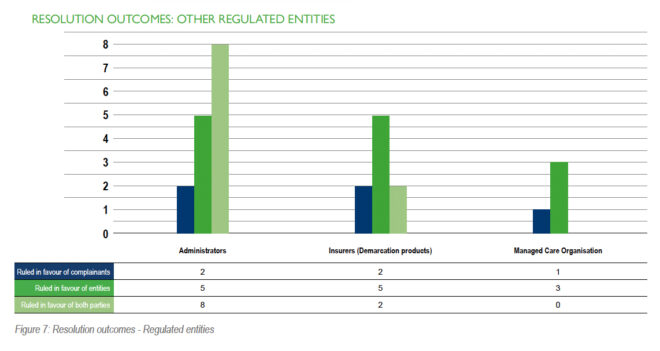
The 1 729 resolved justiciable complaints consisted for 1 701 complaints lodged against medical schemes and 28 complaints lodged against other regulated entities, such as administrators, managed-care organisations, and insurers.
Medical scheme complaints were made up of 1 206 complaints against open schemes and 495 complaints against restricted schemes.
Most complaints relate to administration
The report says the CMS continued to see a higher volume of complaints related to administration. These complaints mainly comprise disputes over the payment of non-statutory benefits for reasons such as benefit exclusions, depletion of benefits, contribution increases, and the imposition of waiting periods.
The CMS resolved 541 complaints about the non-payment and short-payment of Prescribed Minimum Benefits (PMB).
The root causes of disputes over PMB funding include disagreements over the interpretation of PMB levels of care, real or perceived unfairness in the application of treatment protocols and formularies, and short payments related to the use of non-designated service providers.